In a new study conducted by Aclara Research, medical use of cannabis has once again been shown to be a successful substitute for dangerous addictive opioid painkillers for many patients in pain.
The study surveyed over 400 patients and 500 pharmacists to glean their views on the medical use of cannabis and its effect on the use of prescribed opioids.
Sixty-seven percent of the patients surveyed indicated that they were able to cease their use of opioid medications once they had access to a state medical marijuana program. Another 29 percent of the patients were able to reduce their use of opioids, leaving just 1 out of 25 patients (4 percent) whose opioid use was unaffected by marijuana use.
This comports with a study released last year in the journal Health Affairs that showed an average of 1,826 fewer doses of painkillers prescribed annually under Medicare Part D from 2010 to 2013 in the 17 states with a medical marijuana law. Another study in The Journal of Pain found “medical cannabis use was associated with a 64 percent decrease in opioid use” among 244 chronic pain patients in the Michigan medical marijuana program.
More incredibly, 30 percent of the patients surveyed by Aclara indicated they were able to cease use of all prescription drugs after they started using medical cannabis. For the patients who swapped the use of cannabis for prescription pill usage, over 60 percent reported making fewer trips to the pharmacist.
This echoes the findings of another study, published in the National Bureau of Economic Research, that found, ” states permitting medical marijuana dispensaries experience a relative decrease in both opioid addictions and opioid overdose deaths compared to states that do not.”
It’s not the legalization of cannabis for medical use alone that brings about the reductions in opioid addiction and mortality, write the authors, “the mitigating effect of medical marijuana laws is specific to states that permit dispensaries.”
Of the pharmacists surveyed by Aclara, 87 percent agreed that medical use of cannabis should be legal, and 69 percent believe that pharmacists should dispense medical cannabis and counsel patients on its use.
Just 15 percent of the patients indicated that they spoke with their pharmacist about their cannabis use, compared to 40 percent of them who get their information about medical marijuana from the internet and social media.
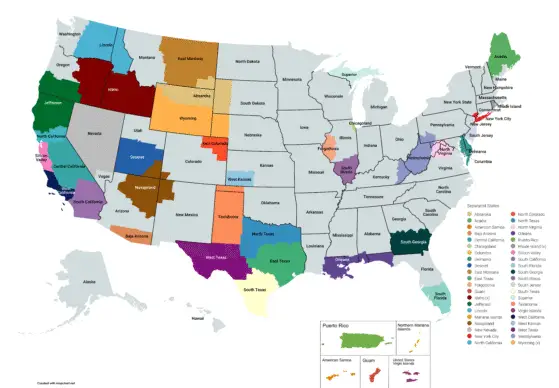
Only five of the thirty states with medical cannabis programs – Minnesota, Pennsylvania, New York, Connecticut, and Arkansas – require pharmacist involvement in medical cannabis dispensaries.
Aclara’s survey is just the latest study to confirm that legal access to cannabis may be our best opportunity to fight back against the ever-growing crisis of drug overdose deaths which have claimed over 60,000 lives in 2016. Overdose death is now the leading killer of Americans under age 50.
Yet President Trump’s commission tasked with finding solutions to the opioid crisis has soundly rejected any increasing access to medical cannabis as a potential solution.
“The Commission acknowledges that there is an active movement to promote the use of marijuana as an alternative medication for chronic pain and as a treatment for opioid addiction,” writes the commission’s chair, outgoing New Jersey Gov. Chris Christie. “Recent research out of the NIH’s National Institute on Drug Abuse found that marijuana use led to a two-and-a-half times greater chance that the marijuana user would become an opioid user and abuser. The Commission found this very disturbing.”
Gov. Christie then proceeds to compare medical marijuana today, after twenty years of existence on the West Coast, to the early days of Oxycontin in the 1990s, when ignorance about its deadly addictive nature was hidden by the corporations pushing this brand-new painkiller.
While his claim about marijuana being a gateway drug to opioid addiction has been debunked for almost two decades now, it’s also irrelevant. What are we going to do for the adults who are already addicted to and dying from these opioid drugs? How does continuing prohibition – which doesn’t stop any kid who wants to from trying pot – help the people dying now under that policy?
We know access to medical cannabis helps.
Way back in 2014, JAMA Internal Medicine published data showing that “states with medical cannabis laws had a 24.8 percent lower mean annual opioid overdose mortality rate compared with states without medical cannabis laws.”
And it’s not some connection to a marijuana dealer that’s leading people to opioid overdoses. It’s a connection to a pharmacist. That 2014 study found about “60 percent of all opioid analgesic overdoses occur among patients who have legitimate prescriptions from a single provider.”
Another study from 2016 in the American Journal of Public Health found that states that implemented a medical marijuana law then saw a 21 percent lower likelihood of detecting opioids in the bloodstream of a driver killed in a car crash. For drivers aged 21 to 40, they were half as likely to find opioids in dead drivers.
That study isn’t making any conclusions about impairment and driving; rather, the idea is that dead drivers are a fairly random sample of the population, so finding fewer of them with opioids in their system may mean that fewer people are taking opioids or taking them less often in the states with medical marijuana laws.
This Aclara survey is just the latest in a growing body of science that shows the Trump Administration’s dedication to reviving failed 1980s drug war policies is precisely the opposite of how we should address the opioid overdose crisis.